3:44
The medical device industry is heavily regulated, for good reason. Expanding your market presence into other geographies comes with its own set of complications as each new device must be approved by each country’s or region’s own regulatory body. For the purpose of brevity, let’s talk solely about the U.S. market and the federal Food and Drug Administration (FDA).
Medical device manufacturers must seek marketing authorization for any new device from the FDA. Depending upon the type of classification assigned to your device, premarket approval may also be required. Every year, the FDA clears approximately 3,000 device submissions with an average turnaround time of 180 days. This can be significantly longer if your device is Class III (devices that support life or are implanted, e.g., pacemakers or breast implants).
Once a submission has been cleared, the approval remains in place for the lifetime of the product. However, if the product has been modified or improved, or you want to change its intended use, you must reapply all over again. As competitors introduce new equivalent devices, you may have no option but to enhance your existing product lines or develop new innovative solutions to keep up. However, your time to market and first-mover status may be significantly affected by this lengthy approval process.
In an attempt to expedite submissions, the FDA created a set of quality regulations that enables them to identify device manufacturers that consistently produce high-quality devices. These regulations help to focus the FDA’s resources on assisting other manufacturers to raise their level of quality, identify and promote practices that support consistent quality manufacturing and align the FDA’s own regulatory, enforcement and compliance approaches with those practices. To implement these quality regulations effectively, medical device manufacturers must therefore rethink their approach to risk and transition from reactive compliance reporting to proactive quality management.
Every medical device manufacturer’s ultimate goal is to improve patient care with safe, effective and high-quality products. However, not every product can be perfect the first time. Indeed, product recalls and litigation are costing the industry billions each year. These recalls are mostly due to production defects and design flaws which could potentially be reduced by adhering to the quality standards set out by the FDA, which recommends that companies implement:
- Design Controls
- Quality Systems
- Production and Process Controls; and
- Documentation Control Procedures
Historically, regulatory workflows and application submissions have been carried out using paper-based systems – a necessary, but significant overhead activity that depletes time, money and resources. These paper-based systems are gradually being replaced by document management and quality management systems, helping to reduce the burden. However, as with all controls and procedures, nothing can be completely automated. These systems are only as effective as the policies, procedures and employee-training programs that you have in place to ensure compliance.
How Design Controls Reduce Production Errors
Integrating effective design controls into your product development workflows enables you to transform regulatory overhead into engineering intelligence, providing critical insights to help you continuously improve both your products and your engineering processes.
Design controls are used to continually assess and provide improved visibility into your product development process to help identify and correct issues earlier. With improved visibility, managers are able to recognize problems, make corrections, and adjust resource allocations. Designers benefit from improved communication and coordination among all stakeholders and get a better understanding of how their intended product conforms to user and patient needs.
Design controls are just one part of a comprehensive quality system that should be used to manage a device from initial requirements through design, production, distribution, use, maintenance, and eventual obsolescence. Although the name suggests that design controls apply only to the initial design of a device, they also apply to any and all changes to the device or manufacturing process, including those occurring long after a device has been introduced to the market. This includes evolutionary changes such as performance enhancements as well as revolutionary changes such as corrective actions resulting from failure analysis. Design changes are necessary to ensure that your medical devices continue to meet the needs of the user or patient.
Therefore, your design control processes must be revisited many times during the life of a product.
Onshape’s latest eBook, “Modern CAD for Medical Device Design,” heavily focuses on Design Controls, specifically how they apply to your use of CAD software and your overall product development process.
Download your copy today and find out what your engineering and manufacturing team is missing!
Latest Content

- Case Study
- Robotics
Saga Robotics: Powering the Future of Sustainable Farming with Cloud-Native Onshape
01.05.2026 learn more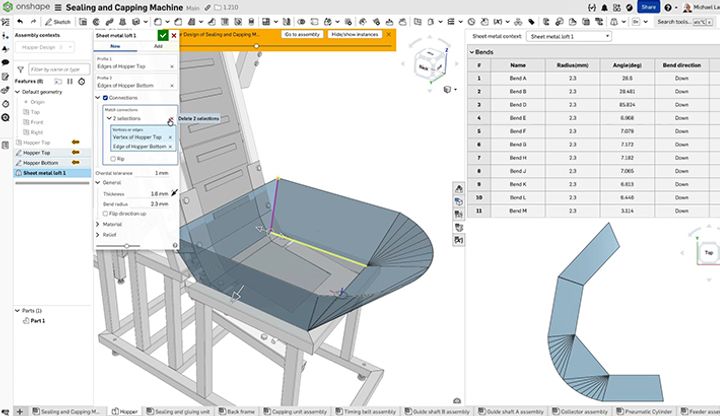
- Blog
- Becoming an Expert
- Sheet Metal
Two Views, One Model: Faster Sheet Metal Design in Onshape
02.12.2026 learn more
- Blog
- Customers & Case Studies
- Collaboration
- Consumer Products
RigStrips Boosts Design Speed Using Onshape's Collaborative Tools
02.11.2026 learn more
- Blog
- Becoming an Expert
- Features
- Data Management
How Onshape's Repair Tool Fixes Broken References
01.29.2026 learn more


